Healthcare Operational Management: A How-To Guide
Behind every smooth patient handoff and well-maintained room is a team working quietly in the background: the healthcare operations and clinical engineering team.
When healthcare operations run efficiently, care is safer, faster, and more reliable. But when gaps appear—missed maintenance, delayed responses, poor coordination—patients and staff feel the impact.
With rising costs and stricter regulations, hospitals can’t afford inefficiencies.
Yet many still rely on outdated systems and technology that slow things down and strain resources.
This blog looks at what healthcare operations management really involves, why conventional approaches fall short, and how smarter systems are helping hospitals deliver better care every day.
What is Healthcare Operations Management?
Healthcare operations management refers to the systems, strategies, and day-to-day processes that keep a healthcare facility functioning safely, efficiently, and in compliance with regulatory standards.
It’s the discipline that ensures every aspect of care delivery—clinical, non-clinical, and facility maintenance—runs in sync.
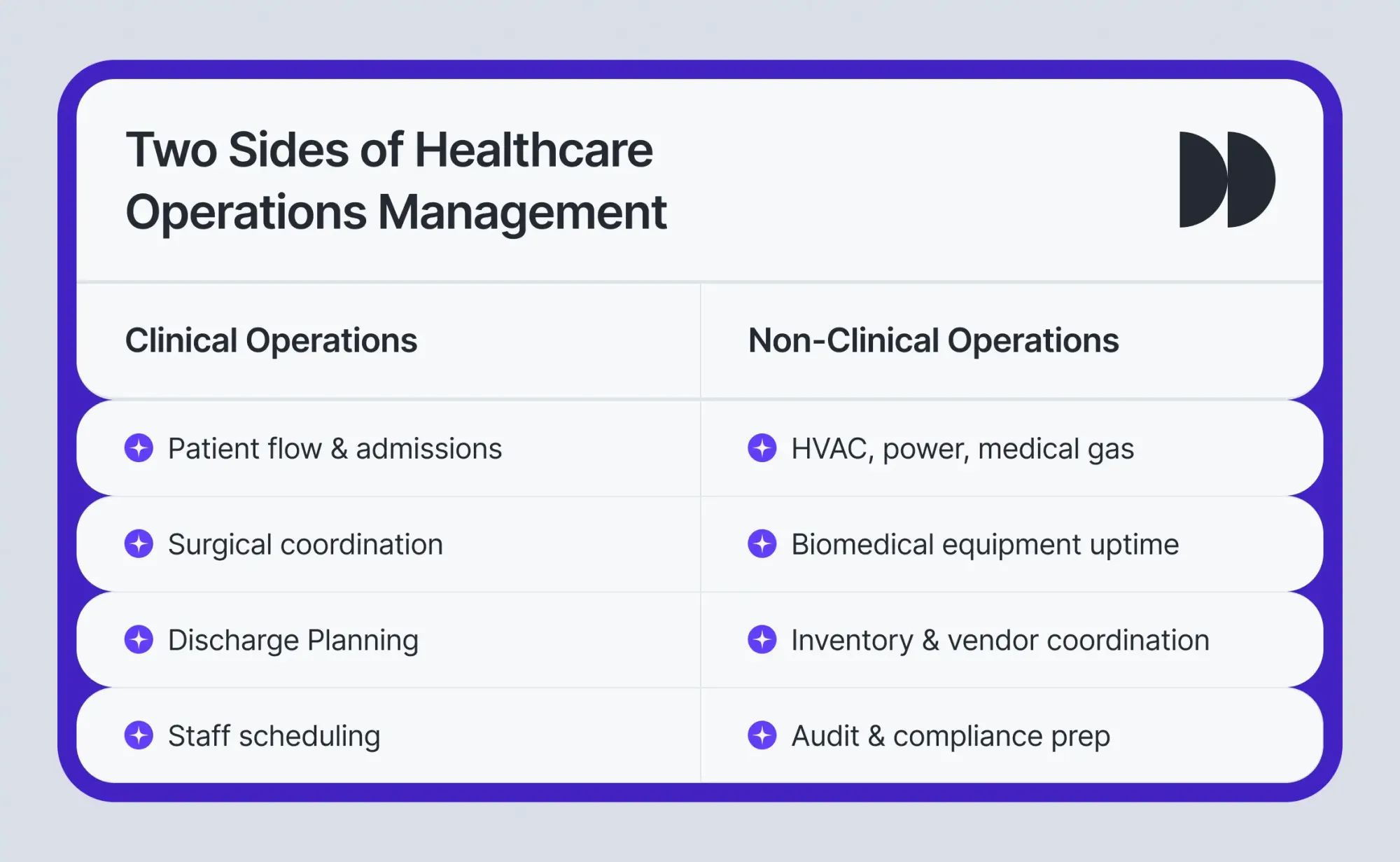
Key areas of focus
- Clinical Operations
- Managing patient flow and admissions
- Coordinating surgical schedules and discharge planning
- Allocating staff and clinical resources effectively
- Ensuring biomedical equipment uptime
- Managing Alternate Equipment Maintenance (AEM) for compliance and reliability
- Ensuring compliance and audit readiness for clinical systems and equipment
- Facility Operations
- Maintaining critical infrastructure (HVAC, power, water, medical gas)
- Overseeing inventory and supply chain logistics
- Coordinating with vendors and contractors
- Preparing for audits and regulatory inspections
- Ensuring facility-wide compliance and audit readiness across systems
Core Objectives
- Prevent care delays and disruptions
- Reduce operational inefficiencies and costs
- Improve safety, satisfaction, and compliance
- Support frontline teams with reliable systems and resources
Who’s involved in HOM?
- Hospital leadership (e.g., COOs, administrators) sets the overall operational goals and performance metrics.
- Operations managers, HTM teams, clinical engineering teams, facilities staff, and procurement teams translate those goals into everyday action—optimizing maintenance, resolving bottlenecks, managing assets, and keeping everything running smoothly behind the scenes.
The role of operations management in today’s healthcare
In today’s healthcare landscape, operational decisions no longer sit quietly in the background. They influence everything—from patient outcomes to financial performance and staff morale.
At its best, healthcare operations management connects clinical teams, facility managers, procurement staff, and administrative teams. It aligns internal departmental processes like patient scheduling, asset management, and regulatory compliance, ensuring seamless communication and coordination across departments.
Here’s how strong operations shape the hospital experience across every level:
1. Improving patient safety and responsiveness
From the moment a patient arrives to the moment they’re discharged, operations influence the quality and speed of care.
For instance, smarter bed use helps reduce emergency room congestion. Coordinated scheduling ensures the right clinician is available at the right time. Behind the scenes, the availability of equipment, cleanliness of rooms, and speed of patient transfers all contribute to delivering care that feels seamless and safe.
2. Removing bottlenecks and improving efficiency
Hospitals today are expected to do more with less. Operations leaders play a critical role in eliminating waste and streamlining workflows. That could mean reducing idle time in surgical suites, ensuring timely equipment maintenance, or breaking down departmental silos through better coordination.
The result is a more agile system where resources are used wisely, and delays are kept to a minimum.
3. Balancing financial health with care quality
Operational excellence isn’t about cutting corners—it’s about spending smarter. By optimizing everything from energy usage and supply inventory to vendor contracts and overtime, hospitals can rein in costs without sacrificing care quality.
In fact, many operational cost savings directly fuel investments in clinical improvements and staff wellbeing.
4. Enabling compliance and smarter decisions
Hospitals generate mountains of operational data—but unless that data is organized, accessible, and actionable, it’s just noise. Strong operations teams ensure that work orders, maintenance logs, and audit trails are captured accurately and used effectively.
This not only helps pass inspections but also empowers leadership to identify trends, fix issues early, and keep the organization future-ready.
Bonus insight: Strengthening staff wellbeing and retention
Good operations don’t just improve care—they reduce chaos.
- When roles are clear, systems work, and issues are resolved proactively, staff feel more supported and less burnt out
- In an industry battling high turnover, smooth operations are a key ingredient in retention
Common challenges in healthcare operations
Operations are the backbone of care delivery. But for many healthcare systems, long-standing inefficiencies still stand in the way of consistent, high-quality performance. These challenges rarely occur in isolation.
Instead, they compound, creating ripple effects that reach from the boiler room to the bedside.
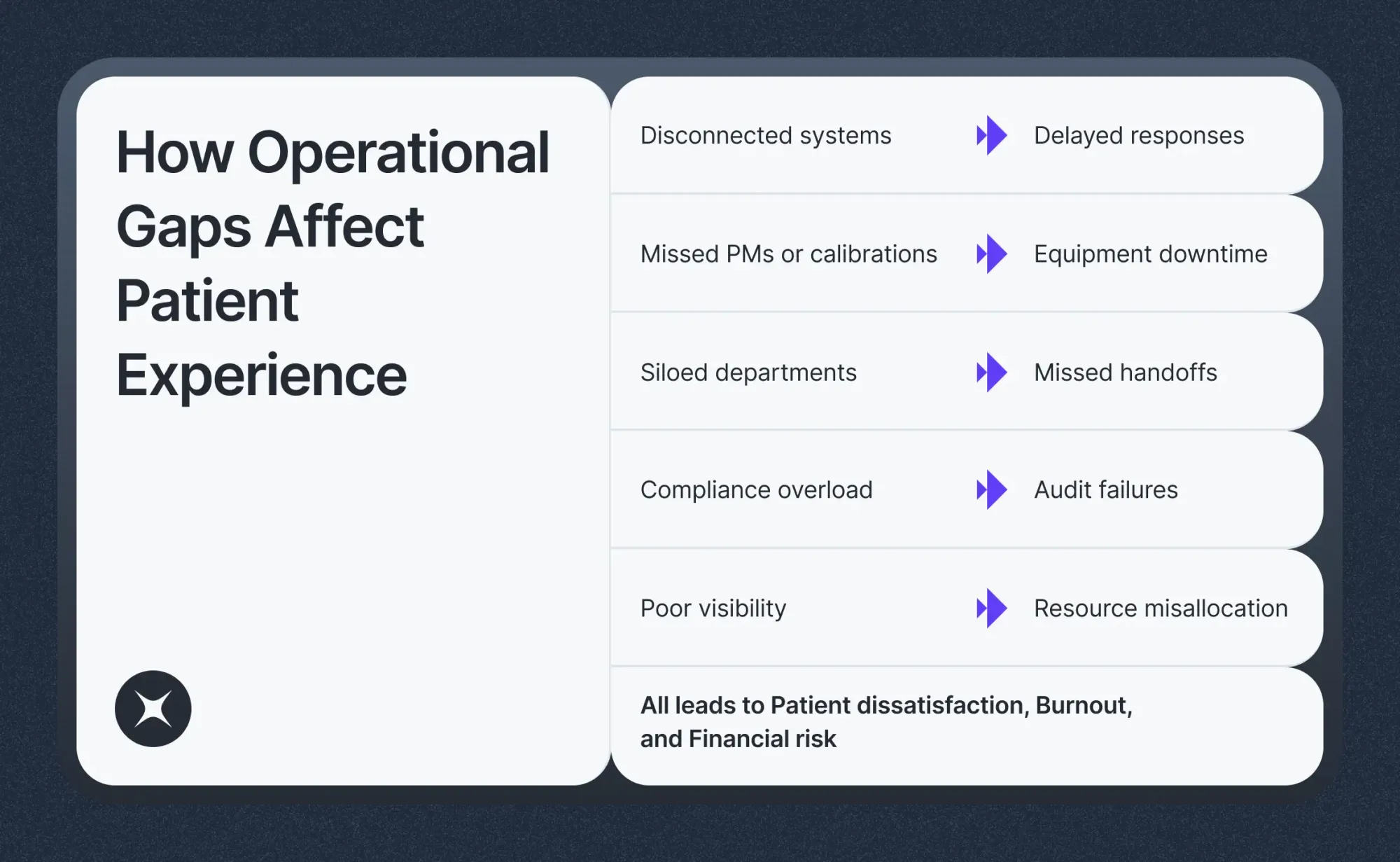
a) Disconnected systems and siloed workflows
Many hospitals continue to rely on outdated tools: spreadsheets, legacy software, or systems that don’t talk to one another.
- Maintenance, clinical scheduling, inventory, and facilities are often managed separately
- Cross-functional visibility is limited or nonexistent
- Teams are stuck reacting to issues instead of proactively resolving them
This leads to delayed responses, duplicated work, and an operations culture constantly playing catch-up.
b) Compliance demands without the infrastructure to support them
Staying compliant isn’t optional—but it’s becoming harder to manage.
- Teams must track inspections, calibrations, and preventive maintenance tasks
- Audits from bodies like TJC, CMS, or OSHA require structured documentation and real-time reporting
Without centralized workflows or automation, staying audit-ready consumes valuable time and increases the risk of missed inspections or penalties.
c) Rising costs, shrinking margins
Operational blind spots are expensive.
- Missed preventive tasks lead to costly equipment failures
- Energy waste and underutilized contracts drain budgets
- Lack of visibility turns minor inefficiencies into long-term losses
When overhead rises faster than revenue, it limits the ability to reinvest in care quality or staff wellbeing.
d) Patient dissatisfaction rooted in operational breakdowns
Patients don’t see the behind-the-scenes systems, but they experience the results.
- Long wait times
- Cancelled procedures
- Delayed discharges
These issues often stem from slow work order response, poor coordination, or inadequate resourcing.
The result?
Eroded trust and lower satisfaction—problems that begin in operations but end at the bedside.
Build a future-ready operations strategy: 6 elements that work
A truly modern healthcare operations strategy doesn’t just fix what’s broken. It equips hospitals to adapt, scale, and stay ahead—whether that means navigating a compliance overhaul, bouncing back from a system failure, or handling an unexpected patient surge.

Here are six elements that high-performing hospitals are using to build operational resilience:
1. Gain real-time visibility into workflows, assets, and performance gaps
Without live insights, hospitals operate on guesswork. A real-time visibility layer helps teams monitor equipment health, track compliance, and spot inefficiencies before they escalate. When everyone sees the same data, decisions get sharper and faster.
2. Standardize processes that flex with regulation and disruption
Rigid protocols break down in crisis. Future-ready hospitals build SOPs that create consistency without sacrificing adaptability. When new mandates arrive or resources shift, your workflows should adjust within hours, not weeks.
3. Deploy no-code, mobile-first tools that teams can use on the ground
Technology shouldn’t slow you down—it should remove blockers. No-code platforms let frontline teams digitize and manage tasks in real time, without waiting for custom IT builds.
The result: faster rollout, better adoption, and fewer silos.
4. Empower staff with smart tools and shared accountability
Training is not enough if systems are clunky or ownership is unclear. Real enablement means intuitive tools, role-based dashboards, and workflows that promote cross-department collaboration.
Everyone knows their part—and who’s got the next step.
5. Turn daily operations into a continuous improvement engine
Quarterly reviews don’t cut it anymore. High-performing hospitals use real-time data to detect bottlenecks, trigger alerts, and refine workflows as they go. These fast feedback loops drive measurable gains without waiting for the next audit.
6. Bridge the gap between facilities, biomed, and clinical care
Operational delays often have clinical consequences. Whether it’s a missed calibration or a discharge stalled by room readiness, siloed teams slow things down. Integrated ops connect the dots—preventing breakdowns before they impact patients.
How Facilio supports excellence in healthcare operational management
Operational excellence in healthcare isn’t just about going digital—it’s about being agile.
Hospitals today need real-time visibility, multi-site coordination, and systems that can evolve as regulations, risks, and priorities change. That’s where Facilio comes in.
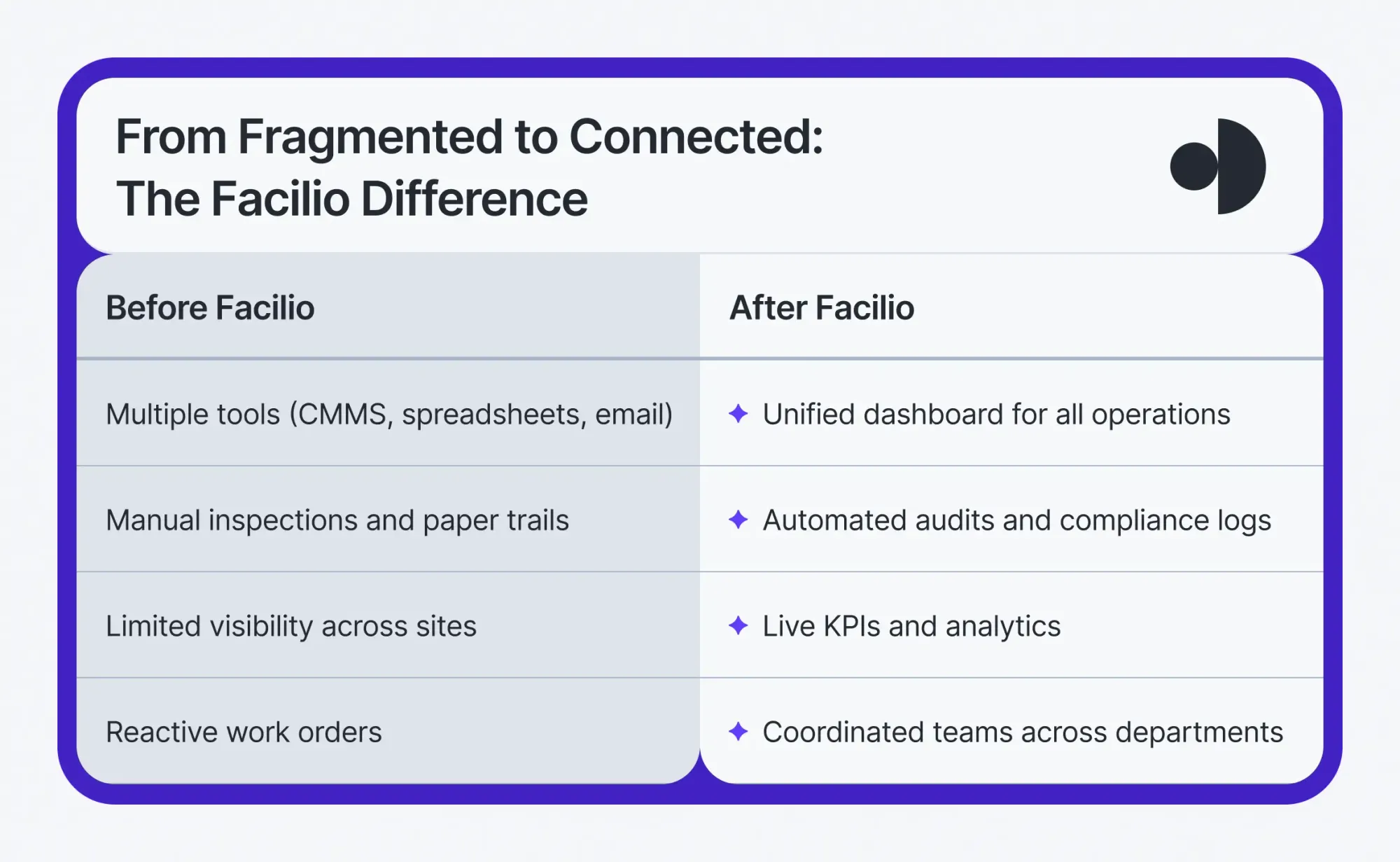
Facilio’s no-code healthcare CMMS software gives hospitals and health systems a single source of truth for managing all of the above, without the complexity of legacy software.
What Facilio enables:
- Centralized visibility across facilities - Monitor assets, compliance, and operations across clinics, hospitals, and remote sites—all in one dashboard.
- Custom KPIs and real-time analytics - Track what matters most: Joint Commission readiness, budget variance, asset lifecycle, vendor response time, or preventive maintenance completion—tailored to your facility type and goals.
- Faster, smarter decision-making - Set up regional command centers, automate work order escalations, and act on live data instead of post-event reports.
- Built-in compliance and audit readiness - Automatically log inspections, calibrations, and PMs. Generate audit trails without the scramble.
- Seamless coordination between departments - Unify facilities, HTM, vendors, and clinical support staff on one connected platform to reduce delays and missed handoffs.
The result:
- Fewer equipment failures
- Higher regulatory scores
- Reduced operational costs
- A more resilient healthcare infrastructure—ready to scale, adapt, and deliver
Listen to what Eurohealth Systems had to say about their experience with Facilio.
“Facilio's Connected CMMS gave our technicians instant visibility — enabling faster resolutions and a smooth shift from reactive to proactive maintenance for one of our largest hospital chains.”
Facilio replaces fragmented tools with a connected ecosystem that lets healthcare leaders control operations with precision and confidence.
Smarter healthcare operations. Better patient outcomes. Seamless coordination at scale.
Discover why forward-thinking hospitals are adopting Facilio’s hospital CMMS to optimize their healthcare operations, enhance efficiency, and improve care delivery across the board.
Upgrade to a Hospital CMMS Built for Compliance and Care
Connected CMMS helps you stay audit-ready, asset-smart, and future-proof — always.

More from Facilio