Understanding Quality Improvement in Healthcare: Frameworks, Examples, and the Role of CMMS
Quality in healthcare is no longer a back-office concern — it’s a frontline priority that directly determines patient outcomes, safety, and trust. Medical errors remain a leading cause of preventable harm, costing health systems billions and undermining patient confidence.
This is where quality improvement (QI) comes into play. It brings structured methods like Lean, Six Sigma, and PDSA cycles to reduce errors and streamline care. Quality management ensures that policies, standards, and compliance frameworks give these efforts direction and accountability. Together, they form the backbone of modern healthcare excellence.
In this guide, we’ll explore the fundamentals of quality improvement in healthcare, the role of quality management, the six domains of healthcare quality, proven frameworks and project examples, and how a healthcare CMMS solution enables organizations to achieve compliance, improve patient safety, and sustain continuous improvement across their facilities.
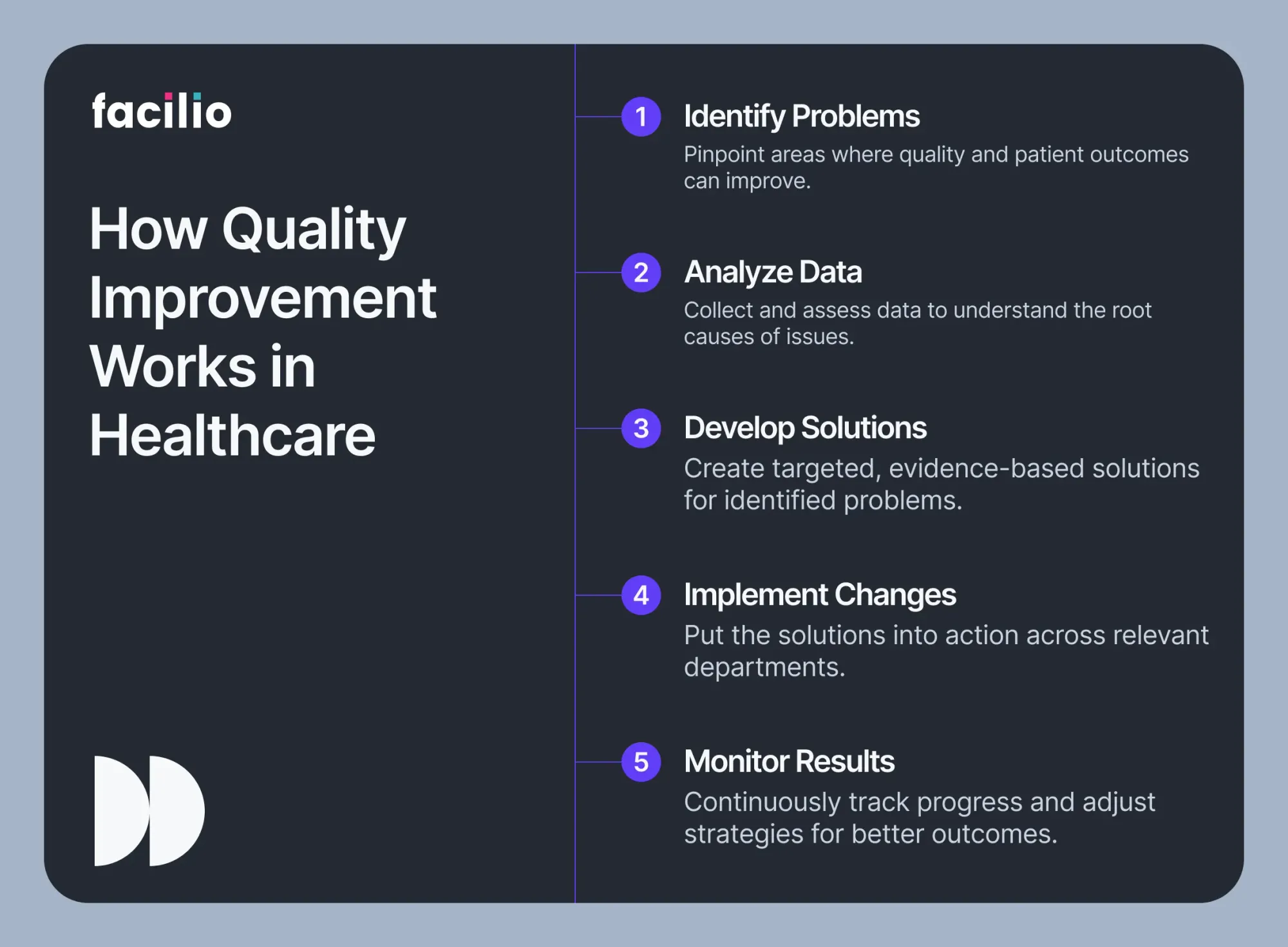
What is quality improvement in healthcare?
Quality improvement (QI) in healthcare is the systematic framework used to raise the standard of care, reduce variation, and create better patient outcomes.
The National Academy of Medicine defines healthcare quality as “the degree to which health services for individuals and populations increase the likelihood of desired health outcomes and are consistent with current professional knowledge.”
Building on this, the Centers for Medicare & Medicaid Services (CMS) describes QI as the process of standardizing structures and processes so that healthcare organizations can achieve predictable, reliable, and safe results.
A landmark report estimated that nearly 98,000 patients die annually due to preventable medical errors in U.S. hospitals, highlighting the urgency of robust QI programs.
Key principles of quality improvement in healthcare include:
- Patient-centered care: Aligning decisions and care plans with patient needs and preferences.
- Evidence-based practice: Using the best available data and research to guide interventions.
- Continuou improvement: Adopting an ongoing, iterative approach to problem-solving.
- Systemic focus: Addressing inefficiencies across teams, processes, and technology—not just individuals.
- Data-driven decision-making: Leveraging performance metrics to identify issues and measure success.
When executed well, it delivers far more than compliance. It improves patient safety and outcomes, reduces operational costs, enhances staff engagement, and strengthens a hospital’s reputation for excellence.
Quality management in healthcare and it’s role in quality imporvement?
Quality management (QM) in healthcare is the structured administration of policies, processes, and system designs that minimize harm, optimize outcomes, and ensure that care consistently meets the highest standards.
While quality improvement drives continuous, day-to-day progress, quality management provides the overarching framework that organizes, standardizes, and sustains excellence across an organization.
Core components of quality management include:
- Quality planning – defining goals, establishing metrics, and creating strategies to meet them.
- Quality control – monitoring processes, identifying errors, and taking corrective action.
- Quality assurance – verifying that services comply with standards and regulations (e.g., Joint Commission, ISO, CMS).
- Quality improvement – embedding lessons from data and feedback into new processes.
Healthcare organizations achieve results by continuously measuring performance, collecting and analyzing data, and adapting processes. Healthcare facility management is critical to bringing this together—standardizing documentation, audits, and reporting.
Quality management and quality improvement are not separate initiatives but two sides of the same coin.
Quality management (QM) establishes the framework—policies, standards, and systems that define what “good care” looks like.
Quality improvement (QI) takes that framework and turns it into action, applying methods like Lean or PDSA to continuously raise the bar.
Without QM, quality improvement efforts lack direction. Together, they create a cycle of governance, measurement, and progress that ensures both compliance and innovation.
Quality management vs. quality improvement in healthcare: At a glance
Quality management ensures healthcare organizations have a strong foundation, while quality improvement ensures they never stop getting better.
The six domains of healthcare quality
The Institute of Medicine (IOM) identifies six domains that define high-quality healthcare: care should be safe, effective, patient-centered, timely, efficient, and equitable.
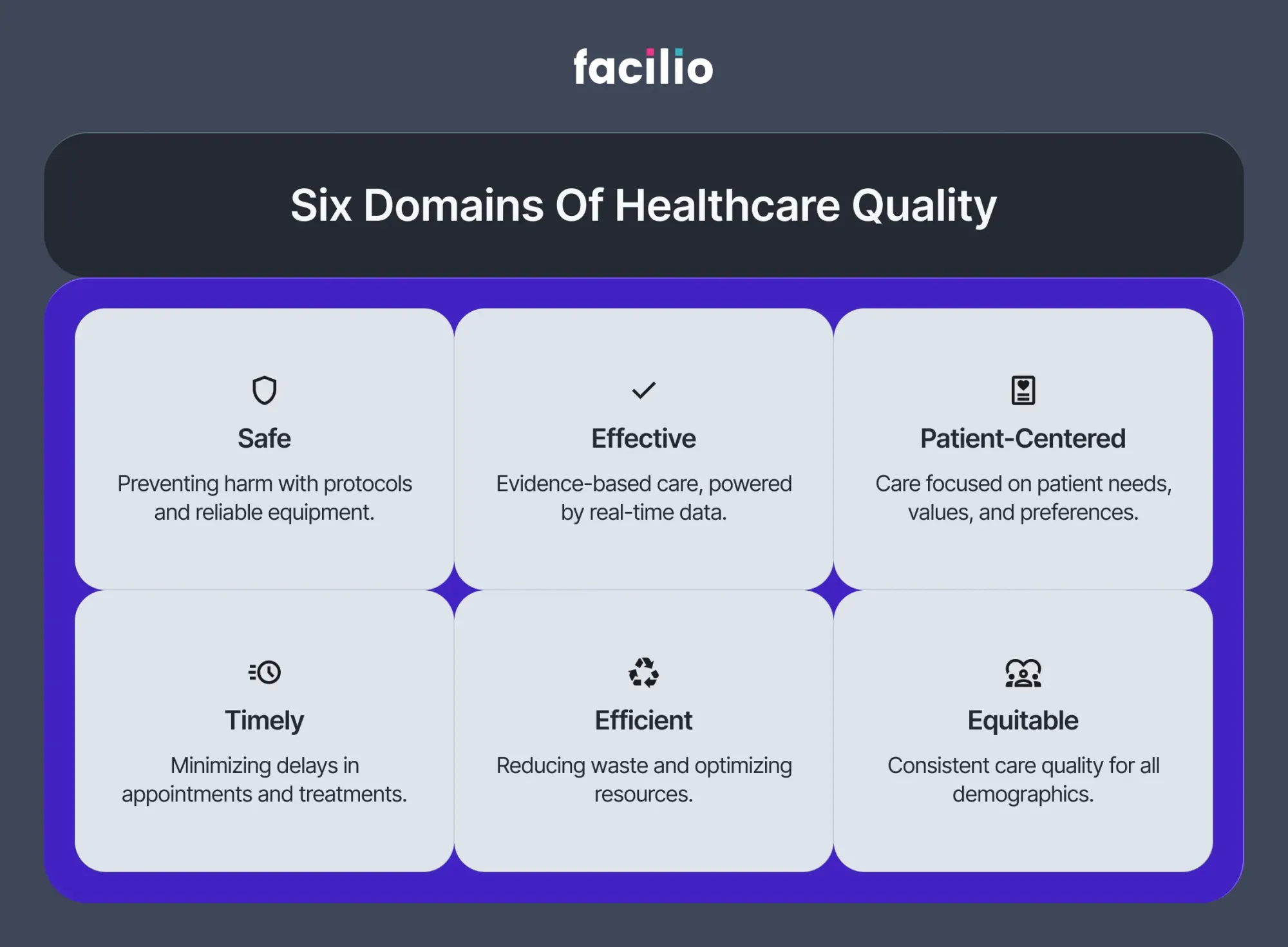
These domains guide both quality management frameworks and quality improvement initiatives, and a modern CMMS provides the operational backbone to make them real.
1. Safe – preventing harm to patients
Care must avoid injuries and medical errors that occur during treatment. Patient safety depends on reliable equipment, sterile environments, and quick responses to hazards.
How CMMS helps: By scheduling preventive maintenance and flagging asset risks in real time, a CMMS reduces the chance of equipment-related incidents. Automated safety checks (e.g., fire alarms, HVAC, sterilization units) ensure clinical spaces remain compliant and hazard-free.
2. Effective – delivering evidence-based care
Care should be based on the best scientific knowledge and delivered consistently. Outdated equipment or unavailable resources can block effective treatment.
How CMMS helps: A hospital CMMS tracks calibration schedules and ensures critical assets—diagnostic machines, ventilators, monitors—are available and accurate when needed. Work orders tied to evidence-based protocols guarantee interventions are carried out under optimal conditions.
3. Patient-centered – respecting patient needs and preferences
Care must honor individual values and provide dignity, privacy, and comfort alongside treatment. Poorly maintained environments or frequent disruptions undermine trust.
How CMMS helps: A CMMS helps facilities maintain clean, safe, and comfortable patient areas by streamlining housekeeping, HVAC, lighting, and room readiness tasks. Patients experience reliable, well-managed spaces that reinforce respect for their needs.
4. Timely – reducing waits and delays
Delays in diagnosis or treatment can worsen conditions and increase stress for patients and providers.
How CMMS helps: A CMMS prevents bottlenecks by keeping diagnostic and therapeutic equipment available through predictive maintenance. When issues do arise, automated work order assignment and real-time mobile updates speed up resolution. This reduces downtime and shortens patient wait times.
5. Efficient – eliminating waste
Healthcare should minimize unnecessary steps, costs, and delays without compromising care.
Automated scheduling and work order prioritization reduce duplicate tasks. Inventory and parts tracking prevent last-minute scrambles. Dashboards reveal underutilized equipment, enabling better resource allocation and cutting operational waste.
6. Equitable – ensuring consistent quality for all patients
Care must be equally accessible and safe, regardless of patient demographics, location, or socioeconomic status.
How CMMS helps: By standardizing asset performance and compliance processes across multiple facilities, CMMS ensures that all patients—urban or rural, insured or uninsured—experience the same quality of environment and equipment reliability.
Frameworks and models for quality improvement in healthcare
Healthcare organizations face complex challenges: rising costs, staff shortages, regulatory demands, and growing patient expectations. Frameworks like Lean, Six Sigma, and the PDSA cycle give providers structured methods to improve care and reduce errors. These models have been widely adopted across hospitals and health systems because they provide repeatable processes for tackling problems and sustaining improvements.
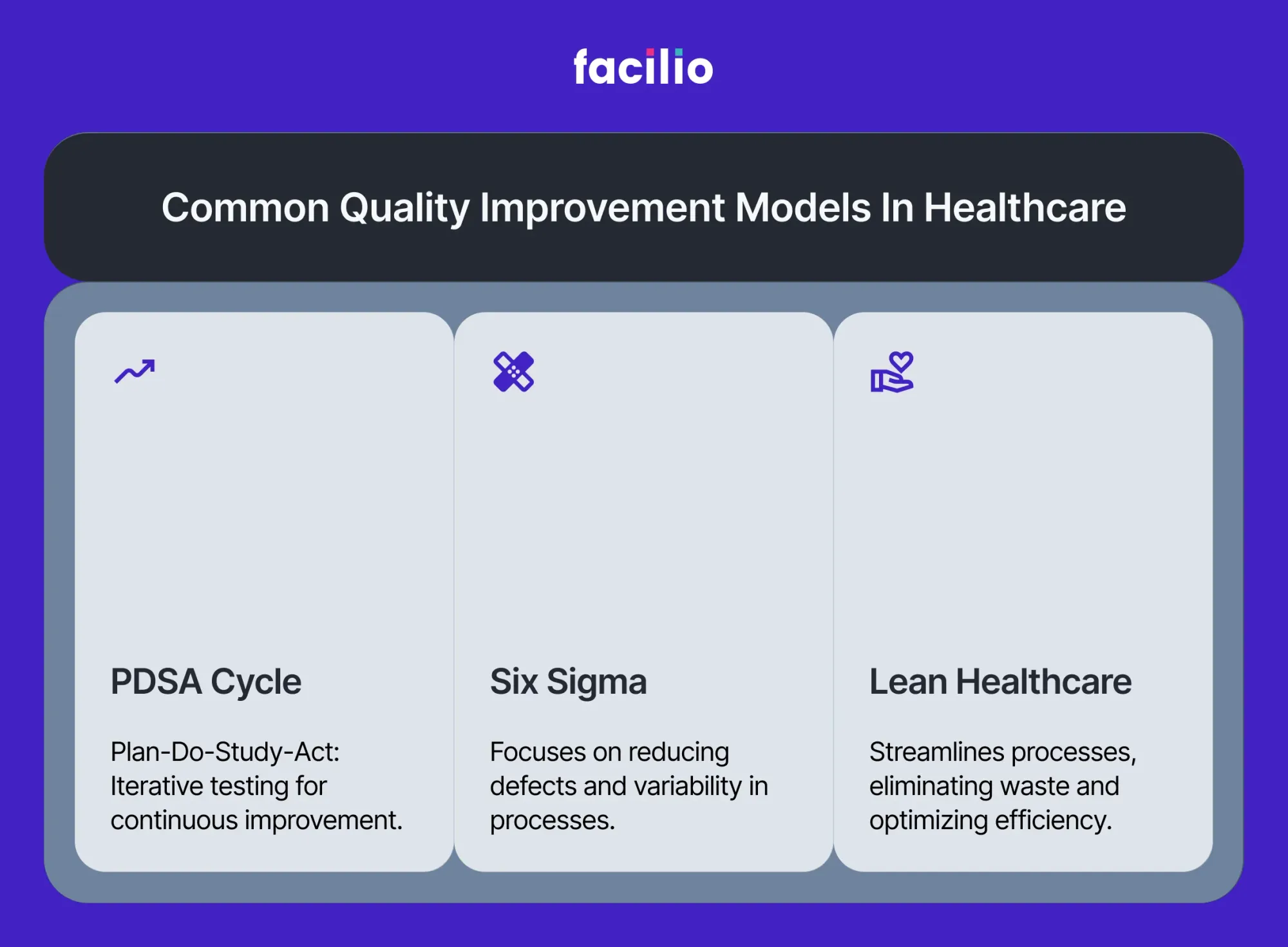
Lean – removing waste to create value
What it is: Originating from manufacturing, Lean focuses on identifying and removing waste—any activity that consumes resources but does not add value to patient care. In healthcare, waste often shows up as long patient waits, repeated diagnostic tests, or unused inventory.
Healthcare application: A hospital might apply Lean to streamline its discharge process. By mapping every step, they may find delays caused by missing prescriptions or last-minute lab work. Simplifying and reordering tasks reduces patient length of stay, freeing beds sooner and improving patient satisfaction.
Six Sigma – reducing errors and variation
What it is: Six Sigma applies statistical analysis to identify and eliminate variation in processes that lead to errors. The goal is consistent, near-error-free performance. In healthcare, variation can mean the difference between safe medication delivery and a preventable adverse event.
Healthcare application: Hospitals often use Six Sigma to address medication errors. By analyzing data on when and how mistakes occur, teams can redesign workflows—such as barcode medication administration or automated pharmacy cabinets—to reduce variability in how drugs are dispensed and administered.
PDSA cycle – testing and scaling change
What it is: The Plan–Do–Study–Act cycle is a simple, iterative model for rapid improvement. Teams plan a change, implement it on a small scale, study the results, and then act by either adopting, adapting, or abandoning the change.
Healthcare application: A care team might test a new protocol for reducing hospital-acquired infections in one ICU unit. They monitor infection rates over a month, study the data, and, if successful, roll out the protocol hospital-wide.
Other essential tools
Beyond Lean, Six Sigma, and PDSA, healthcare organizations often rely on additional QI tools:
- Root Cause Analysis (RCA): Investigates why an adverse event happened to prevent recurrence.
- Failure Mode and Effects Analysis (FMEA): Identifies where a process or piece of equipment might fail and prioritizes risks before they occur.
- Statistical Process Control (SPC): Uses data charts to monitor processes and detect variation over time.
These frameworks give healthcare teams a disciplined way to improve quality, reduce errors, and enhance efficiency. Lean tackles waste, Six Sigma reduces variation, and PDSA enables fast learning and adaptation.
How CMMS supports these frameworks: A CMMS strengthens them all by supplying the operational data, automation, detailed logs of asset failures, response times, and compliance checks that improvement models depend on.
Examples of quality improvement in healthcare
Quality improvement comes to life when theory translates into measurable outcomes for patients and providers. Across hospitals and health systems, projects often target the most pressing challenges: safety risks, inefficiencies, and preventable harm. Here are some real-world examples.
1. Reducing hospital-acquired infections (HAIs)
Infections acquired during hospital stays increase morbidity and cost. Hospitals combat HAIs with stricter sterilization protocols, hand-hygiene audits, and improved ventilation in ICUs and operating rooms.
2. Improving medication safety
Medication errors remain one of the most frequent preventable harms. Barcode administration systems and double-check protocols help ensure patients receive the correct drug and dose.
3. Enhancing discharge planning
Uncoordinated discharges often lead to confusion and readmissions. Teams now use discharge checklists, patient education, and follow-up calls to improve continuity of care.
4. Reducing readmissions
High readmission rates affect both patient outcomes and reimbursement. Predictive analytics and stronger post-discharge support programs target at-risk patients.
5. Advancing healthcare equity
Quality improvement also addresses disparities in access and outcomes. Initiatives focus on expanding preventive care, engaging with underserved communities, and monitoring equity metrics.
How CMMS powers quality management and improvement in healthcare
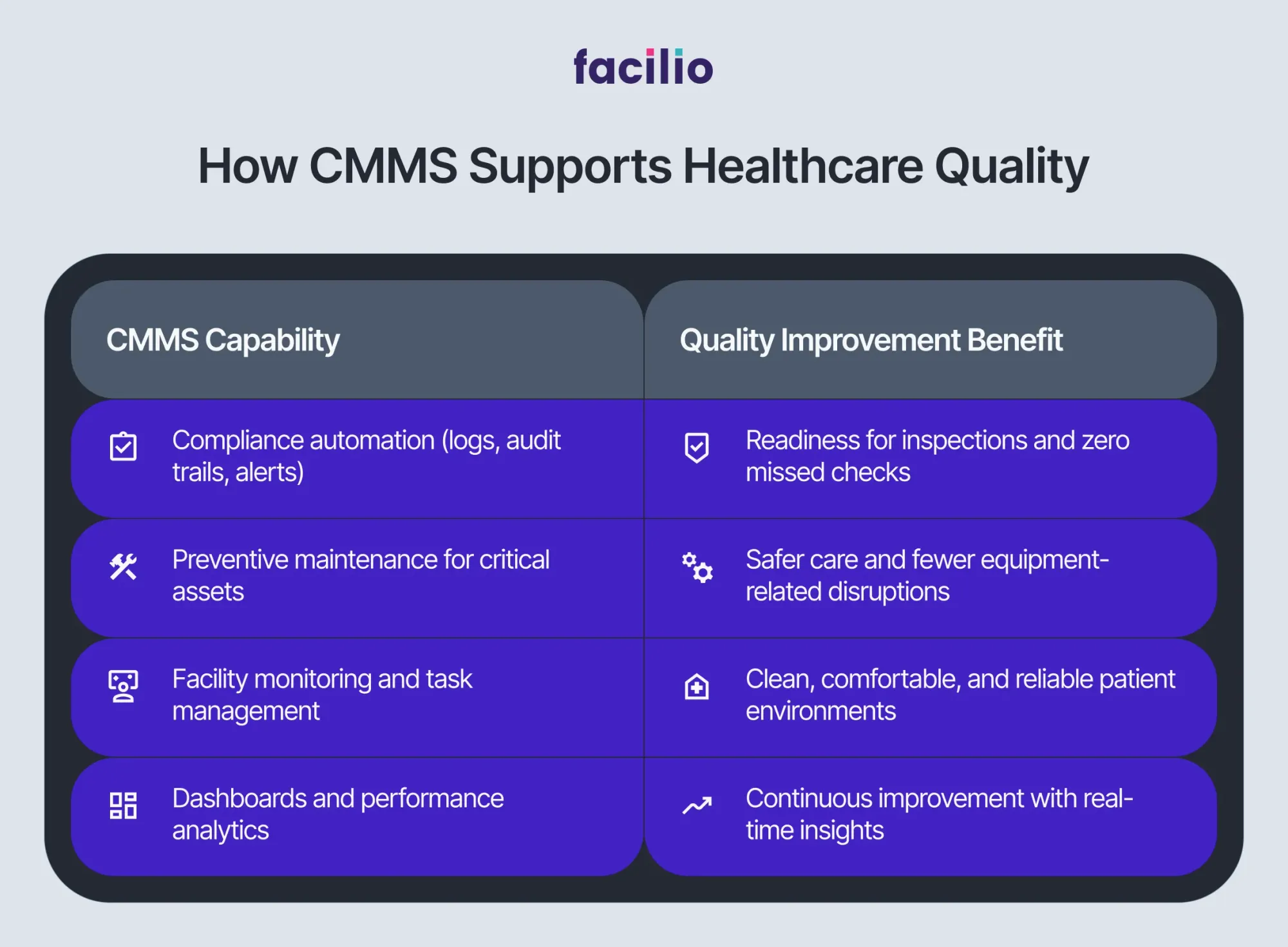
No matter how strong a hospital’s policies or improvement initiatives are, quality depends on reliable operations. Equipment failures, missed compliance checks, or environmental breakdowns can quickly derail patient care and undermine progress. A healthcare CMMS solution bridges the gap between clinical quality goals and day-to-day execution, ensuring safety, efficiency, and compliance across the entire facility.
1. Compliance and accreditation readiness
Regulatory bodies like The Joint Commission require strict documentation of safety checks, maintenance schedules, and corrective actions.How CMMS supports compliance:
- Automates compliance logging for critical systems.
- Provides digital audit trails, making inspections faster and error-free.
- Flags overdue tasks to prevent gaps that risk joint commission compliance.
2. Asset reliability and patient safety
Healthcare depends on the availability of diagnostic, therapeutic, and life-safety equipment. When assets fail, delays and safety risks follow. How CMMS supports asset reliability:
- Tracks usage and maintenance history of every device in a healthcare asset tracking system.
- Enables preventive maintenance to minimize downtime of critical assets like MRI machines, ventilators, or infusion pumps.
- Provides real-time visibility so staff can reroute or schedule resources without delay.
3. Facility performance and patient experience
A safe, comfortable, and reliable environment is inseparable from quality care. Poor air quality, broken HVAC, or delayed room turnovers directly affect patient outcomes.How CMMS supports facilities:
- Monitors HVAC, fire safety, and environmental systems.
- Streamlines housekeeping and room readiness workflows.
- Ensures that healthcare facility management teams can deliver consistent, patient-centered environments across all sites.
4. Driving continuous improvement
QI projects succeed only when frontline data is available. Without reliable metrics, it’s impossible to measure whether an intervention is working.How CMMS drives QI:
- Centralizes work orders, asset data, and safety checks for analysis.
- Supports Lean, Six Sigma, and PDSA by tracking process changes and their outcomes.
- Offers dashboards that highlight bottlenecks, failure trends, and cost drivers—turning operational data into actionable improvement strategies.
A CMMS makes compliance transparent, keeps assets reliable, supports patient safety, and powers continuous improvement initiatives. In modern healthcare, technology isn’t just supporting quality—it’s defining it.
Proven impact and outcomes of quality improvement enabled by CMMS
When quality management and improvement are embedded into daily operations, the impact is visible across every dimension of healthcare delivery.
Hospitals with strong QI programs report fewer adverse events, lower readmissions, and higher patient satisfaction.
When combined with modern CMMS technology, the outcomes are numerous:
- Patient safety: Reduced harm events through reliable equipment and proactive maintenance.
- Clinical outcomes: Lower infection rates, reduced readmissions, and shorter lengths of stay.
- Staff engagement: Frontline teams spend less time troubleshooting broken systems and more time caring for patients.
- Financial performance: Fewer penalties, higher reimbursement, and lower operational costs (maintenance costs drop 18–25% with CMMS data-driven scheduling).
- Reputation and trust: Compliance success, positive patient reviews, and awards tied to measurable quality metrics.
The future of healthcare quality
The next era of healthcare quality will depend on real-time intelligence. Hospitals are moving beyond retrospective audits toward systems that predict risks and optimize outcomes before issues occur.
- Predictive analytics: AI models use CMMS data to forecast equipment failures and prevent downtime before it disrupts care.
- Connected quality dashboards: Integrating clinical and operational metrics in a single view helps leaders track safety, performance, and compliance simultaneously.
- Sustainability as quality: Energy efficiency and environmental monitoring, powered by CMMS, ensure facilities are both safe and sustainable.
- Continuous adaptation: As new standards and regulations emerge, CMMS platforms make it easier to update protocols and cascade changes across every site instantly.
Healthcare quality technology isn’t just about meeting today’s standards—it’s about creating systems that adapt, predict, and continually improve. By combining structured quality management with continuous improvement methods, and powering both through a connected CMMS, healthcare organizations can deliver safe, effective, patient-centered care that stands the test of time.
Frequently asked questions (FAQs)
1. What is an example of a quality improvement project in healthcare?
Examples of quality improvement projects in healthcare include reducing hospital readmissions through better follow-up care, preventing infections with stricter safety protocols, and improving patient flow by streamlining discharge or diagnostic processes. These initiatives cut costs, raise patient satisfaction, and improve outcomes.
2. What are the five components of quality improvement?
The five components of quality improvement in healthcare are:
- Design and Scope – broad-based, organization-wide QI design.
- Governance and Leadership – accountability and culture of safety.
- Feedback, Data Systems, and Monitoring – reliable data to track quality.
- Performance Improvement Projects (PIPs) – focused initiatives to tackle priorities.
- Systematic Analysis and Systemic Action – root cause analysis and system-wide fixes. (source)
3. What are the five D’s of healthcare quality?
Healthcare quality indicators often cluster around the 5 D’s: Death, Disease, Disability, Discomfort, and Dissatisfaction. These represent the critical areas healthcare systems must minimize through robust QM and QI programs.
4. What are the four steps of quality improvement?
The widely used PDSA cycle outlines four iterative stages: Plan, Do, Study, and Act. Teams plan a change, test it in practice, study the results, and refine or expand based on evidence.
5. What is the most common method of quality improvement used in healthcare?
The Plan-Do-Study-Act (PDSA) cycle is the most widely used approach. It enables rapid-cycle testing of small changes, making it a practical tool for frontline staff and leadership to drive continuous improvement.
6. What are the seven principles of quality management?
According to ISO 9001, the seven principles are: Customer focus, Leadership, Engagement of people, Process approach, Improvement, Evidence-based decision making, and Relationship management. These guide organizations in building effective quality management systems.
7. What are the four main components of quality management?
The four pillars are:
- Quality Planning – setting objectives and requirements.
- Quality Assurance – ensuring compliance with standards.
- Quality Control – monitoring outputs to detect errors.
- Continuous Improvement – ongoing refinement of processes. (source)
8. What are the three C’s of quality in healthcare?
The “3 C’s” framework emphasizes Consistency, Continuity, and Coordination in heathcare delivery. Together, these ensure patients receive seamless, reliable, and integrated healthcare experiences.
More from Facilio