Featured healthcare CMMS
Healthcare Facilities Management: Strategy, Challenges & Smart Tools
Ever thought about where most of a hospital’s money goes?
When people think of hospital budgets, they picture new wings or advanced medical tech. But the real backbone of care is the facility itself, and keeping it running takes constant investment.
From HVAC and power systems to sterilization and safety equipment, operations and maintenance ensure patient care never gets interrupted.
In healthcare, smooth facility performance isn’t optional — it’s critical.
That’s where healthcare facilities management (HFM) comes in.
It’s the team working quietly behind the scenes to make sure hospitals, clinics, and care centers are safe, compliant, and always ready.
Whether it’s fixing equipment, maintaining clean air systems, or preparing for emergencies, HFM is what keeps the lights on — literally and figuratively.
But in the U.S., this job is getting harder.
Aging buildings, rising costs, and tighter regulations — all while patients expect seamless care. Teams need to do more, with less, and do it faster.
This blog breaks down:
- What modern HFM really looks like
- Why it’s more important than ever
- And how to level up with practical strategies and smarter tech (like healthcare CMMS platforms)
By the end, you’ll walk away with clear ideas you can act on — whether you’re running a large hospital or a small care center.
What is Healthcare Facilities Management (HFM)?
Healthcare Facilities Management (HFM) refers to the specialized coordination of all physical aspects of a healthcare environment to ensure it remains safe, functional, and compliant.
In simpler terms, HFM keeps hospitals and healthcare facilities running, so that doctors, nurses, and patients don’t have to worry about what’s happening behind the scenes.
Unlike general facility management, HFM in hospitals requires strict adherence to the Joint Commission standards and regulations. So, it’s not just about maintaining a building — it’s about creating an environment that protects lives.
What does HFM include?
HFM covers a wide range of responsibilities, including:
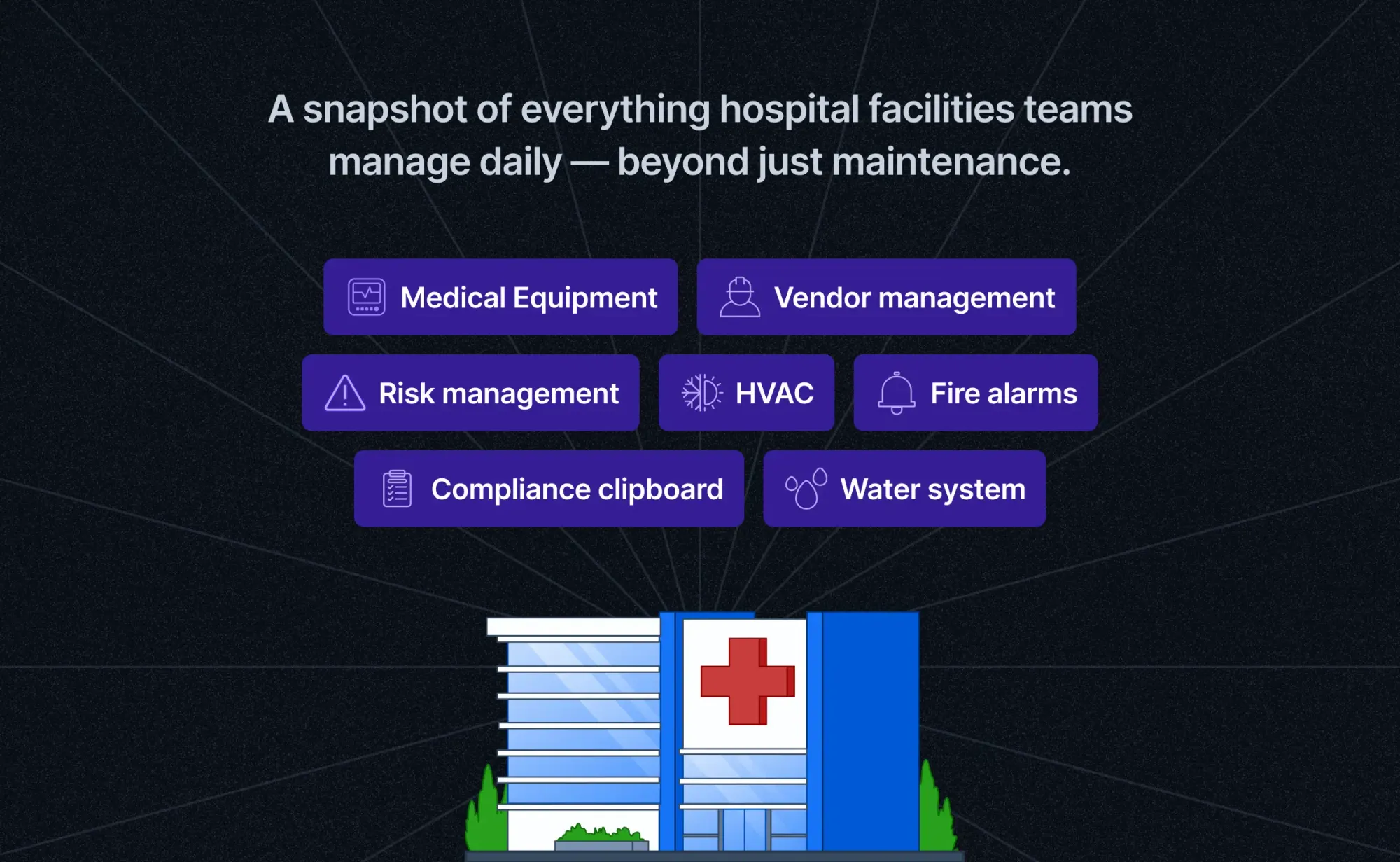
- Hospital maintenance of both medical and non-medical equipment
- Oversight of healthcare building systems like HVAC, emergency power, fire alarms, and water filtration
- Infection control and environmental safety
- Regulatory compliance (HFM compliance USA) — including Joint Commission, OSHA, and state-specific codes
- Security systems and emergency response planning
- Vendor management and facility service contracts
- Data and asset tracking through hospital facility management software
How is HFM different from general facility management?
While general facility management may apply to schools, offices, or commercial properties, hospital facilities management demands a higher level of precision and accountability.
Here’s how HFM stands apart:
That’s why healthcare facility teams rely on specialized tools like purpose-built hospital CMMS, deep industry knowledge, and precision workflows to get the job done right, every single time.
What are the responsibilities of a healthcare facility manager?
Healthcare facility managers play a key role in making sure hospitals stay safe, efficient, and ready to support patient care at all times.
Their work isn’t just about fixing things—it’s about ensuring the whole hospital runs smoothly, meets standards, and stays future-ready.
Here are the core responsibilities every hospital facility management professional must master:
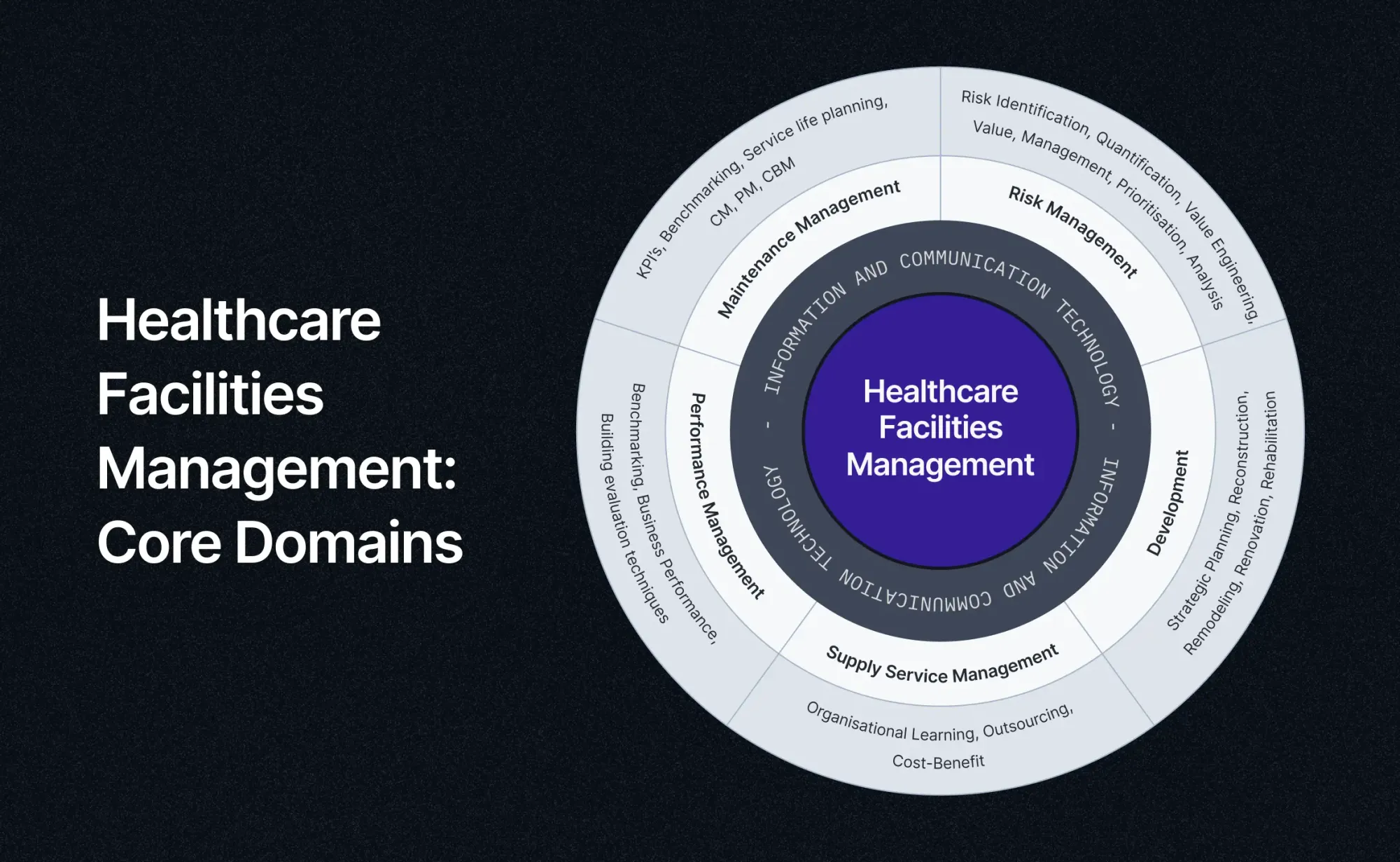
1. Maintenance management: keeping assets operational and safe
A hospital’s infrastructure—HVAC systems, water supply, medical gases, sterilization equipment, and elevators—must operate flawlessly 24/7. Any failure can jeopardize patient care and safety.
Key responsibilities:
- Lifecycle planning: Forecasting the expected lifespan of assets and scheduling timely replacements to avoid sudden breakdowns.
- Maintenance mix: Balancing corrective (CM), preventive (PM), and increasingly important condition-based maintenance (CBM) strategies to reduce unplanned downtime and costly emergency repairs.
- Benchmarking & KPIs: Defining measurable performance indicators for maintenance efficiency, asset utilization, and energy performance.
2. Performance management: Aligning operations with care delivery goals
Facility managers must ensure the building performs in line with clinical and operational targets, such as infection control, patient comfort, and staff productivity.
Key Responsibilities:
- Building Performance Audits: Regular assessments of indoor air quality, lighting, temperature, and energy efficiency—factors that directly affect patient recovery rates and staff well-being.
- Sustainability benchmarks: Implementing green building standards, energy management, and water conservation measures to reduce environmental impact and operational costs.
- Operational efficiency: Streamlining processes to minimize waste, optimize space utilization, and improve service delivery.
3. Risk management: Safeguarding life, compliance, and reputation
The hospital environment is filled with risks, including power outages, fire hazards, the spread of infections, and equipment failure. Effective risk management ensures the continuous delivery of care.
Key Responsibilities:
- Risk Identification & Prioritization: Conducting hazard analysis for building systems, identifying vulnerabilities, and ranking them by severity.
- Emergency preparedness: Ensuring backup power, fire suppression, evacuation plans, and infection control measures are robust and tested.
- Value management: Balancing risk mitigation efforts with cost considerations to ensure compliance without overspending.
4. Supply Services Management: Enabling non-clinical support functions
From laundry and waste disposal to kitchen services and janitorial staff, non-clinical services keep the hospital clean, safe, and functional.
Key Responsibilities:
- Vendor Oversight: Managing contracts and SLAs for outsourced services to ensure hygiene, food safety, and operational reliability.
- Cost-Benefit Evaluation: Identifying areas where outsourcing is beneficial versus in-house management.
- Organizational Learning: Training staff on safety protocols, waste handling (especially biohazardous material), and green practices.
5. Development & Infrastructure Planning: Preparing for the future
Hospitals must evolve to meet changing healthcare demands—more ICU beds, better air handling, expanded emergency services.
Key Responsibilities:
- Strategic Planning: Aligning facility upgrades with clinical expansion plans, patient volume forecasts, and technology adoption (like robotic surgery units).
- Renovation & Retrofitting: Leading projects for remodelling or rehabilitating aging infrastructure to maintain competitiveness and regulatory compliance.
- Sustainability Integration: Incorporating green building design (LEED, IGBC) into new developments to future-proof the hospital.
Insight: Facility managers are not just operational heads—they influence hospital growth, long-term cost savings, and environmental stewardship.
6. ICT Integration: The Digital Backbone of Modern Facilities
Technology is transforming facility management—from real-time energy dashboards to IoT-connected medical devices.
Key Responsibilities:
- CMMS & BMS Integration: Running advanced maintenance platforms and Building Management Systems to automate asset tracking, fault detection, and energy management.
- Data Analytics: Using performance data to drive decisions, predict failures, and optimize resource use.
- Cybersecurity: Protecting building systems (HVAC, lighting, elevators) from cyber threats—an emerging but overlooked risk.
Managing too many tasks across tools?
Switch to a CMMS that connects your team, data, and decisions.
Schedule a Demo NowWhat are the challenges in healthcare facilities management?
Managing healthcare facilities today isn’t just hard — it’s high stakes.
In the U.S., facility managers juggle a complex mix of responsibilities that impact patient care, safety, operations, and compliance.
The first step to staying ahead?
Understanding the biggest challenges — and knowing how to tackle them with the right strategies and tools.
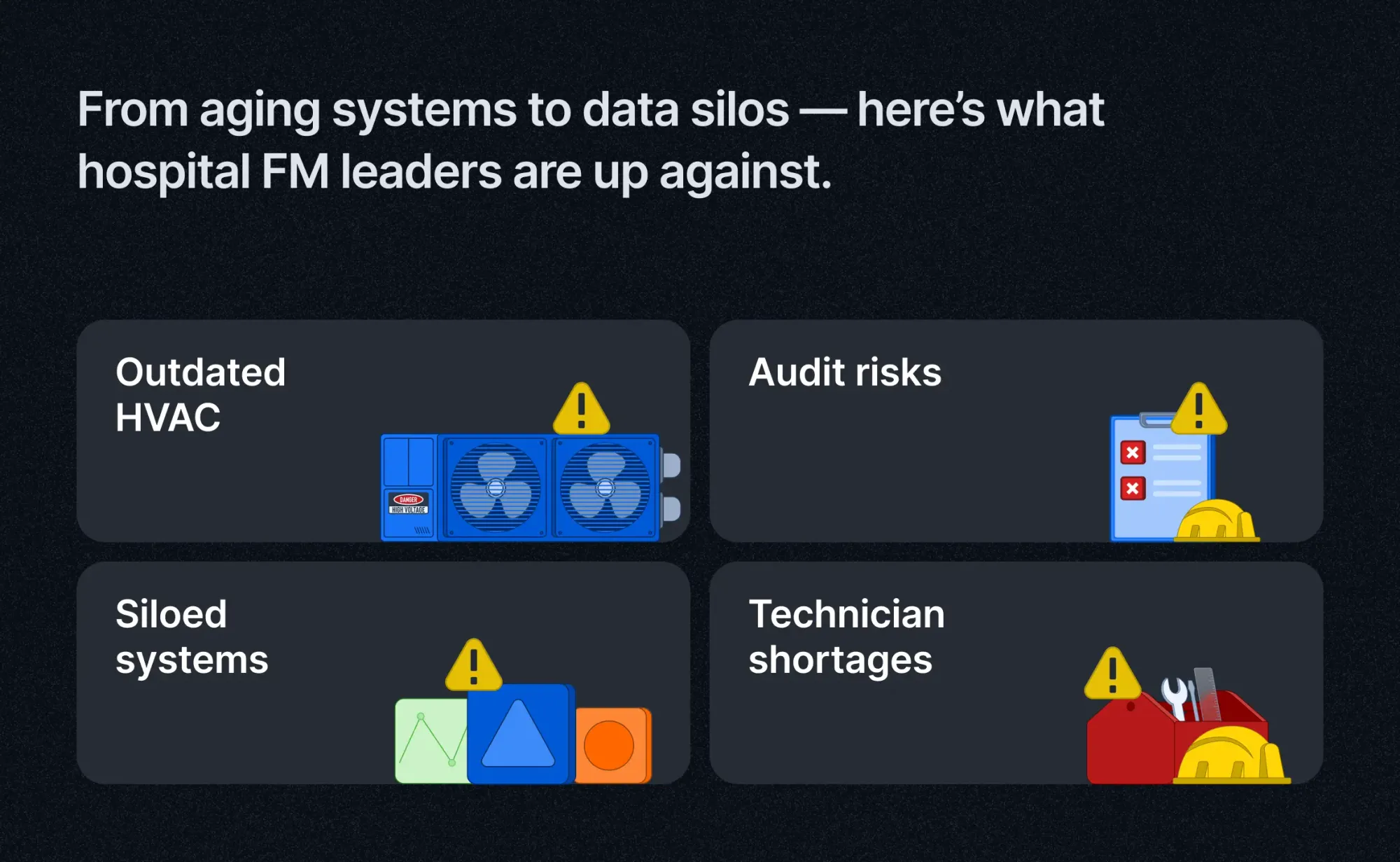
1. Dealing with aging infrastructure and obsolete systems
Many US hospitals and healthcare facilities operate with decades-old buildings and systems. Outdated HVAC units, plumbing, electrical wiring, and medical equipment increase the risk of failure, costly repairs, and inefficiencies.
This makes hospital infrastructure maintenance a critical ongoing priority — one that demands proactive investment and careful lifecycle management.
2. Keeping up with evolving regulatory and compliance demands
The regulatory landscape for healthcare facilities is constantly evolving, with agencies like the Joint Commission, OSHA, NFPA, and ASHE tightening requirements.
Failure to meet HFM compliance USA standards can result in hefty fines, legal risks, and damage to the hospital's reputation. Staying audit-ready requires rigorous documentation, training, and continuous improvement efforts.
3. Lack of real-time asset visibility and control
Without an integrated hospital facility management software, tracking the status, maintenance history, and location of critical assets is difficult. Siloed spreadsheets or disconnected systems delay response times and can lead to equipment downtime, safety risks, and inefficient workflows.
4. Escalating energy costs from inefficient building operations
Hospitals rank among the highest energy consumers due to 24/7 operations and energy-intensive systems. Managing energy effectively is essential to reduce operational costs and meet sustainability goals.
However, legacy systems and limited data visibility often prevent healthcare facilities from achieving optimal energy management and sustainability.
5. Shortage of skilled facility management professionals
The healthcare facility management workforce faces shortages of skilled technicians, engineers, and compliance experts. This limits the ability to perform preventive maintenance, respond to emergencies, and implement new technologies. Training and retaining qualified personnel remain ongoing challenges.
6. Disconnected systems and data silos hindering decision-making
Many hospitals struggle with fragmented facility management systems that don’t communicate with each other.
This siloed data environment hinders collaboration, impedes real-time decision-making, and reduces the effectiveness of hospital maintenance programs.
How to build an effective healthcare FM strategy
In today’s high-stakes healthcare environment, waiting for things to break isn’t an option. Reactive maintenance doesn’t just drain budgets — it can put patient safety at risk.
A modern, proactive approach to healthcare facilities management ensures that your assets remain reliable, your compliance remains airtight, and your care is never interrupted.
Here’s a step-by-step framework to help you build a future-ready hospital facility management strategy that’s built for resilience, efficiency, and long-term success.
1. Conduct a comprehensive facility audit
Start by understanding what you have.
A facility audit helps document your current infrastructure, assess asset conditions, and identify gaps in compliance, safety, or performance. This step is essential for risk mitigation and capital planning.
2. Prioritize critical assets for patient safety and operations
Not all equipment is equal. Categorize assets based on their impact — from life-saving devices and HVAC systems to generators and fire suppression. This allows your team to focus on what matters most and schedule preventive hospital maintenance accordingly.
3. Set clear KPIs to measure success
Metrics matter. Define performance indicators such as equipment downtime, work order resolution times, energy usage, and compliance readiness. These KPIs create accountability and drive data-backed improvements across your healthcare facility operations.
4. Train internal teams and external vendors
Technical skill gaps can lead to preventable errors.
Regularly train your in-house maintenance staff and contracted vendors on SOPs, compliance updates, and safety protocols. This ensures consistency, especially in high-risk environments like ORs and ICUs.
5. Establish feedback loops and reporting systems
Encourage a culture of continuous feedback.
Make it easy for technicians, nurses, or department heads to report issues, track progress, and escalate critical needs. Regular reporting helps facility managers identify patterns and optimize resource allocation.
6. Choose the right CMMS software — your most critical decision
Of all the steps above, selecting the right CMMS for healthcare is where strategy becomes execution.
Why?
Because without a modern, connected hospital facility management software, everything else falls short.
For instance, a Connected CMMS acts as your digital command center, tracking every asset, automating compliance, assigning work orders, and generating real-time insights. It replaces siloed spreadsheets, paper logs, and guesswork with one unified platform tailored for healthcare.
With the right solution, you can:
- Automate preventive maintenance across medical and non-medical systems
- Achieve real-time visibility into asset health, technician performance, and regulatory readiness
- Cut energy waste and unplanned downtime
- Create audit trails that are always inspection-ready
- Scale operations across multiple sites — without scaling your headaches
A modern CMMS doesn't just make your job easier. It elevates hospital facilities management from reactive firefighting to proactive care, aligned with both clinical and operational goals.
Meet the CMMS that’s built for hospitals, not just buildings
Everything we’ve covered — from reducing downtime and improving energy efficiency to staying audit-ready and scaling across sites — depends on one critical factor: the system you use to manage it all.
Most CMMS platforms are designed for buildings.
But Facilio hospital CMMS is purpose-built for hospitals.
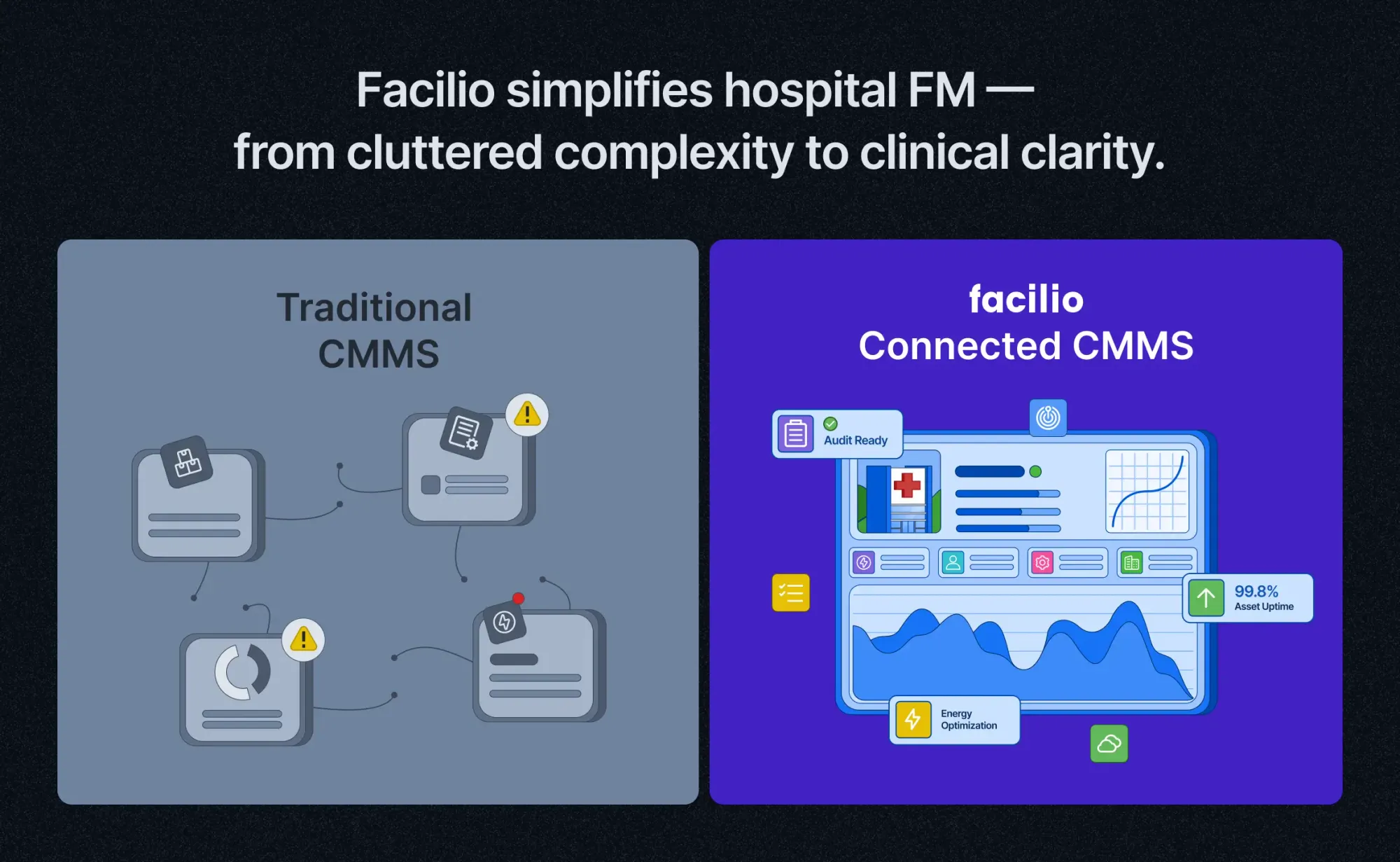
It’s more than just a tool — Facilio is a connected, cloud-based platform purpose-built to handle the complexity of healthcare facilities. It goes beyond tracking work orders to help you:
- Create safer care environments
- Maintain continuous compliance
- Align facilities performance with clinical priorities
Hospitals across the globe are already seeing the impact of modern, purpose-built healthcare CMMS platforms.
Why leading hospitals choose Connected CMMS for healthcare facilities management
Facilio goes beyond traditional CMMS platforms designed for general buildings. It's built from the ground up for healthcare—designed to handle the complexity, compliance, and criticality of hospital environments.
Listen to what Eurohealth Systems had to say about their experience with Facilio.
“Facilio's Connected CMMS gave our technicians instant visibility — enabling faster resolutions and a smooth shift from reactive to proactive maintenance for one of our largest hospital chains.”
Here’s how Facilio can work wonders for you—just like we did for Eurohealth:
✅ Hassle-free compliance, always audit-ready: Automate regulatory audits, track every inspection, and stay aligned with Joint Commission, OSHA, NFPA, and ASHE standards — without last-minute scrambles or paperwork overload.
✅ Multi-site visibility from a single dashboard: Oversee all your hospitals, outpatient clinics, long-term care centers, and specialty facilities through a single command center. Track assets, processes, and performance metrics in real time—no matter the location or facility type.
✅ Regional command centers with full control: Set up centralized hubs to manage healthcare facility operations at scale. Gain granular insights on energy use, biomedical equipment uptime, budget utilization, and compliance performance—tailored to each facility’s unique needs.
✅ Clinical-grade uptime and asset performance: Proactively maintain HVAC, sterilization systems, emergency power, and biomedical equipment to prevent failures that could disrupt patient care. Real-time alerts help you address risks before they escalate into non-compliance or downtime.
✅ No-code customization for healthcare workflows: Easily configure inspection templates, preventive maintenance routines, and emergency protocols—without relying on IT teams or third-party vendors.
✅ Unified platform for people, processes, and biomedical systems: Centralize operations, connect your teams, and integrate medical and non-medical systems across the entire network—eliminating silos and manual effort.
Smarter operations. Safer patient care. Total control at scale.
See why forward-thinking hospitals are switching to Facilio’s CMMS to power smarter operations and better care.
Upgrade to a Hospital CMMS Built for Compliance and Care
Facilio helps you stay audit-ready, asset-smart, and future-proof — always.






